Last Friday was International Overdose Awareness Day, a time to raise awareness and combat stigma related to drug overdose and addiction. I’m not sure whether it’s the industry we’re in, or the way my brain’s wired, but it made me think about if and what can be transmitted through breast milk, and just what effect could it have on that little human that’s dependent on you.
I decided to break-up my research into three components:
- Infections
- Medications
- And Recreational drugs
Firstly, the big spoiler: Yes, there is definite evidence that some drugs and infectious diseases can pass through breastmilk and affect your child. I’m sure that’s not really a surprise, but knowledge is always good for assessing these potential dangers, and mitigating as much risk to your child as possible.

Infectious Diseases
Let’s start with infectious diseases, and whether or not you should be breastfeeding. Before we start, it’s worth stating that if you are concerned, you should certainly discuss your medical history with your doctor or your baby’s pediatrician.
It is extremely rare for a mom to need to stop breastfeeding for illness as there are only a few very serious illnesses that might require a mom stop breastfeeding for an extended period of time or permanently, but the Centers for Disease Control and Prevention (CDC) do outline breastfeeding ‘blackout’ times around treatment for a larger number of infections.
Let’s start with the more common, ‘every-day’ illnesses such as a cold, sore throat, flu, gastroenteritis (rotavirus & norovirus), fever, mastitis, etc. you should continue to breastfeed. In fact, breastfeeding is proven to play an important role in the immune protection of breast-fed infants against NV. Just remind your doctor you are nursing so that if medications are needed he can prescribe something that is compatible with breastfeeding – more on this later.
Let’s move on to the less-common infections, but where more care must be taken to ensure infections are not transmitted


Chicken pox (Varicella): If the infection began within five days before giving birth or two days afterward avoid direct contact with your baby – though it’s okay to use expressed milk. After this period, breastfeeding is safe.
Syphilis & Herpes simplex: Herpes and syphilis can be passed on to the infant if mothers have an active infection, but breastfeeding is considered safe as long as the infection is considered inactive, or you don't have lesions on your breast. To be clear, you can breastfeed as long as your baby or pumping equipment does not touch a sore, but it is advised to use a breast pump or hand express your milk until breast sores heal. Please remember that risks of transmission are increased with an active infection, and if parts of your breast pump touch the sores while pumping, you should throw the milk away.
Hepatitis: With Hepatitis A, breastfeeding is safe. With Hepatitis B, breastfeeding is also safe, although your baby should receive a dose of hepatitis B immune globulin (HBIG) and the first of three doses of hepatitis B vaccine soon after birth. Hepatitis C virus may be transmittable through breast milk, but it is not certain. However, bleeding or cracked nipples on the breast of a woman with Hepatitis C puts a breastfeeding infant at higher risk for getting the virus.
Infectious Tuberculosis: Breastfeeding is safe after you've undergone treatment for at least two weeks and you're no longer contagious.
Cytomegalovirus (CMV): Breastfeeding is usually safe, but check with your pediatrician. The virus can pass to the baby through your milk and, in very rare cases, lead to health problems – especially in preterm infants or babies with extremely low birth weight.
Leprosy (Hanson’s Disease), Lyme Disease, Malaria, Mumps, or Rubella (German Measles): Breastfeeding is considered safe. If you do contract measles and are contagious at the time of birth, you may need to be separated from your baby for a few days to reduce the chance of infection. If this is necessary, express your milk and feed it to your baby until you are no longer contagious and can resume nursing. A few cases of leprosy in infants have been reported where infection may have occurred during breastfeeding, but these reports date prior to the introduction of MDT, when secondary dapsone resistance was common. Women should be advised not to withhold breastfeeding, whether for fear of harm to the child from MDT or for fear of infecting the child with leprosy.
HIV and AIDS: With HIV infection, breast-feeding increases the risk of maternal-fetal transmission by about 25% with late breast-feeding (after six months of age) constituting a particular risk. Quite simply, the CDC advise mothers in the United States who are infected with HIV not to breastfeed, since the virus may be passed in the breast milk to their infant.
Chlamydia, Gonorrhea, or HPV Breastfeeding is considered safe.
Chronic Illnesses: Women with illnesses including Cystic Fibrosis, Diabetes, Epilepsy, Multiple Sclerosis (MS), Thyroid issues, cardiac problems, and High Blood Pressure can almost always breastfeed. While medications associated with each illness need to be considered, the general rule is that if you can and want to breastfeed, then you should – it will be absolutely beneficial to your child. While I limit this discussion to specifically the transmittal concerns through the act of breastfeeding, the folks over at Breast Feeding Basics give far more detail on the issues associated and suggestions to help that actual act of breastfeeding with these conditions.
Allergies: Symptoms of an allergy to something in the mother's diet include diarrhea, rash, fussiness, gas, dry skin, green stools with mucus, or the baby pulling up his/her knees and screaming. This doesn't mean the baby is allergic to your milk - if you stop eating whatever is bothering your baby, the problem usually goes away on its own. It takes about two to six hours for your body to digest and absorb food and pass it into your breast milk, so if your baby shows any of the symptoms above, think about what you ate two to six hours ago. To be sure if those foods are causing the problem, you will have to eat them again and see if he/she has the same reaction. Sometimes a baby can be born with a condition called primary lactase deficiency or with galactosemia, in which they can't tolerate breast milk. This is because their bodies can't break down lactose, a sugar found in the milk of humans and animals. Symptoms include diarrhea and vomiting. Babies with severe galactosemia may have liver problems, malnutrition, or mental retardation. Babies with these conditions must be fed formula that comes from plants, such as soy milk or a special galactose-free formula.

Cancer: a breastfeeding mother cannot pass on cancer to a child as cancerous cells cannot be passed to the baby through breastmilk. If you are undergoing chemotherapy or radioactive isotope therapy, you will need to stop breastfeeding. Resume again when your doctor tells you that the radioactive elements or medications are completely flushed out from the body.
Diagnostic Procedures: X-rays, Ultrasounds, Mammograms and CAT scans are non-invasive procedures that should not affect your breast milk A Fine-needle aspiration cytologic study should not interrupt breastfeeding. MRI (magnetic resonance imaging) is a non-invasive technique that will not in itself affect your breast milk, however, as part of the procedure, you may be injected with a dye that may or may not be transmittable through breast milk, so if you are concerned you can discard the milk pumped after the procedure. Consult a knowledgeable health care provider for specifics on how long to wait before resuming breastfeeding.
Brucellosis can be transmitted via breastmilk. In the acute phase of the disease in the mother, breastfeeding should be avoided, but the use of expressed and pasteurized human milk is allowed. Breastfeeding may be restored as soon as the disease is treated with antimicrobials and the nursing mother shows clinical improvement.
Chagas' disease Studies show that Trypanosoma cruzi can be isolated in human milk in acute and chronic forms of Chagas' disease, but the risks are so low that the disease is considered not transmissible from mother to child through breast milk, and mothers who have the disease can safely breastfeed their babies. Mothers can be treated, but they must wait until after they have stopped breastfeeding because the drugs used to treat Chagas disease are contraindicated in women who are pregnant or breastfeeding.

Medications
Most medications have not been tested in nursing women, and there is no definitive answer to exactly how a given drug will affect a breastfed child. Most over-the-counter and prescription drugs, taken in moderation and only when needed, are thought to be safe. You should always check first with a health care provider before taking medicine.
To reduce the baby's exposure, you can take the drug just after nursing or before the baby sleeps. Even mothers who must take daily medication for conditions such as epilepsy, diabetes, or high blood pressure may be able to breastfeed.
The folks over at Breast Feeding Basics have some general guidelines for taking drugs while nursing :
- Only take a medication if you really need it. Consider alternative, non-drug therapies if possible.
- If you have a choice, delay starting the drug until the baby is older. A drug which might cause problems for a newborn may be fine for an older, larger, more mature infant.
- Take the lowest possible dose for the shortest possible time.
- Avoid drugs with long-half lives, sustained-release preparations, or high M/P (milk to blood) ratio. If the M/P ratio is one or higher, that means that more of it is transferred into the milk.
- Schedule the doses so that the lowest amount gets into the breast milk (take it soon after a feeding, preferably a night feeding, rather than right before nursing).
- Watch for reactions such as sleepiness, rashes, diarrhea, colic, etc. Although reactions are rare, it is important to keep your doctor informed of any changes.
- If you must take a drug that is contraindicated, and no alternatives are available, get a good electric pump to maintain your milk supply if you need to wean for more than a day or two. Your supply will build up when the baby starts nursing again.
Some very general information about drugs that are usually considered safe to take during breastfeeding follows:
- If the drug is commonly prescribed for infants, it is most often safe to take while nursing, because the baby generally gets a much lower dose from the milk than he would from taking it directly. Examples are most antibiotics, such as amoxycillin.
- Drugs considered safe during pregnancy are usually, but with a few exceptions, safe to take while nursing. When you’re pregnant, medication that gets into your bloodstream has a direct line from mom to baby through the placenta; when you’re breastfeeding, drugs that enter your bloodstream are filtered through the breast, and less gets into your milk.
- Drugs that are not absorbed from the GI tract (stomach or intestines) are usually safe. Many of these drugs are injected, such as heparin, insulin, lidocaine, or other local anesthetics. Immunizations such as German measles, flu shots, TB tests, or Hepatitis A and B, are not harmful to the baby – even the ones with live viruses. Topical medications (those applied to the skin) are nearly always safe because they don’t enter the bloodstream.
In general, when breastfeeding it is considered safe to take:
- Acetaminophen (like Tylenol)
- Antibiotics
- Antacids and digestive aids
- Lact-Aid, Lactobacillus acidophilus, Tums (also a good source of calcium), and Tums E-X or Ultra, Mylanta or Mylanta extra-strength, Mylicon, Maalox, DiGel, Gaviscon, Alka-Seltzer, Phazyme, Rolaids, and Tagamet.
- Artificial Sweeteners
- Saccharin and Splenda (sucralose) are not known to cause any problems in nursing moms.
- Aspartame (Equal or NutraSweet) is safe unless your baby has PKU, a very rare metabolic disorder which every baby should be screened for soon after birth – ask your doctor if you’re not sure.
- Cough, Cold, and Allergy Preparations
- Try to use single ingredient, short acting forms of the drug.
- Epilepsy medications (although one, Primidone, should be taken with caution - talk with your health care provider about this drug)
- Sore throats
- Avoid lozenges and sprays which contain phenol, or hexylresorcinols. (These include Cepastat, Listerine, and Sucrets lozenges, and Vicks Chloraseptic Sore Throat Spray).
- Instead, choose Celestial Seasonings, Cepacol Lozenges, NICE Lozenges, and Vicks Lozenges – these contain menthol/and/or benzocaine rather than phenols
- You can also use Sucrets Lozenges if they contain dyclonine rather than hexylresorcinols.
- Sinus congestion
- Pseudoehpedrine is a nasal decongestant which is considered safe, as very little of it is excreted into breastmilk.
- If you want to use a nasal spray to relieve sinus congestion, the majority of them are safe.
- Look for preparations that contain sodium chloride, oxymetazoline, or phenylephrine (such as Afrin, Breathe Free, or Dristan, or Neo-Synephrine).
- Avoid those containing propyhlexedrine (Benedrex). desoxyephedrine (Vicks Vapor Inhaler), or Lemetamfetamine (Nuprin Cold Relief Inhalor).
- Most antihistamines
- Aspirin (should be used with caution)
- (Salicylate) is not recommended for use during pregnancy or lactation due to the small risk of Reye’s syndrome in infants and while it is very unlikely that its occasional use would cause a problem, it’s better to avoid if possible.
- Decongestants for coughs o Robitussin, Mucinex, Triaminic Expectorant, and Vicks Nyquil are not known to be harmful, but watch for infant drowsiness.
- Expectorants like Guaifenesin (the main ingredient in Mucinex, Robitussin, Benylin) don’t suppress coughs. They loosen up the mucus in the respiratory tract to make it easier to cough up. They haven’t been known to cause any adverse effects in nursing babies, but they also don’t seem to be very effective.
- Avoid multi-action formulas such as Tylenol Multi-Symptom Cough medication and Vicks Nyquil Liquid or Liquicaps.
- Dextromethorphan is an antitussive/cough preparation that seems to work by elevating the cough threshold in the brain. It’s the main ingredient in Benylin and Robitussin DM. It’s considered to be the safest of the antitussives, and the one least likely to transfer into milk.

- Ibuprofen (like Advil)
- Insulin
- Quinine
- Thyroid medicines
- Progestin-only birth control pills (the "mini-pill")
- For constipation
- Use formulations containing pysillium, docusate, methylcellulose,or magnesium hydroxide (Citrucel, Colace, Fiberall, Fibvercom, Maalox Daily Fiber, Metamucil, Mylanta, Philips’ Milk of Magnesia, Serutan, or Surfak.
- Avoid those containing mineral oil, phenolphthalein, bisacodyl, and castor oil (Correctol, Dulcolax, Ex-Lax, Feen- a-Mint, Peri-Colace, and Senokot). These may cause stomach upset in the baby.
- Most sleep preparations
- Nytol QuickCaps, Sleep-Eze, Sominex Formala 2, and Unisom Maxium Sleepgels, are ok.
- Avoid those which contain doxylamine, (such as Nytol Maximum Strength, and Unisom), and always watch for excessive sleepiness in your baby.
- For nausea and vomiting:
- Benadryl, Emetrol, and Dramamine are usually safe.
- Again, watch for drowsiness, and try to take the dose after you nurse.
- Avoid compounds containing meclizine or cyclizine, such as Bonine, Dramamine II, and Marezine.
- Most weight control products
- Such as Acutrim and Dexatrim contain phenylpropanolamine and large amounts of caffeine. While there is no data on transmission via breast milk, it is best to avoid them.
- All the major hemorrhoid preparations
- Such as Americaine, Anusol, Nupercainal, Preparation H, and Tucks gel or pads are safe to use while breastfeeding.
You can go to the American Academy of Pediatrics web site, for a more detailed list of drugs and their effect on breast milk.
Keep in mind that all of the OTC medications approved for use in nursing mothers are very safe, and in nearly all cases, the risk of side effects on your baby is extremely small. Due to concerns about liability, many health care providers are going to err on the side of caution, just in case. This doesn’t mean that taking a decongestant or an antacid or a cough drop is dangerous.
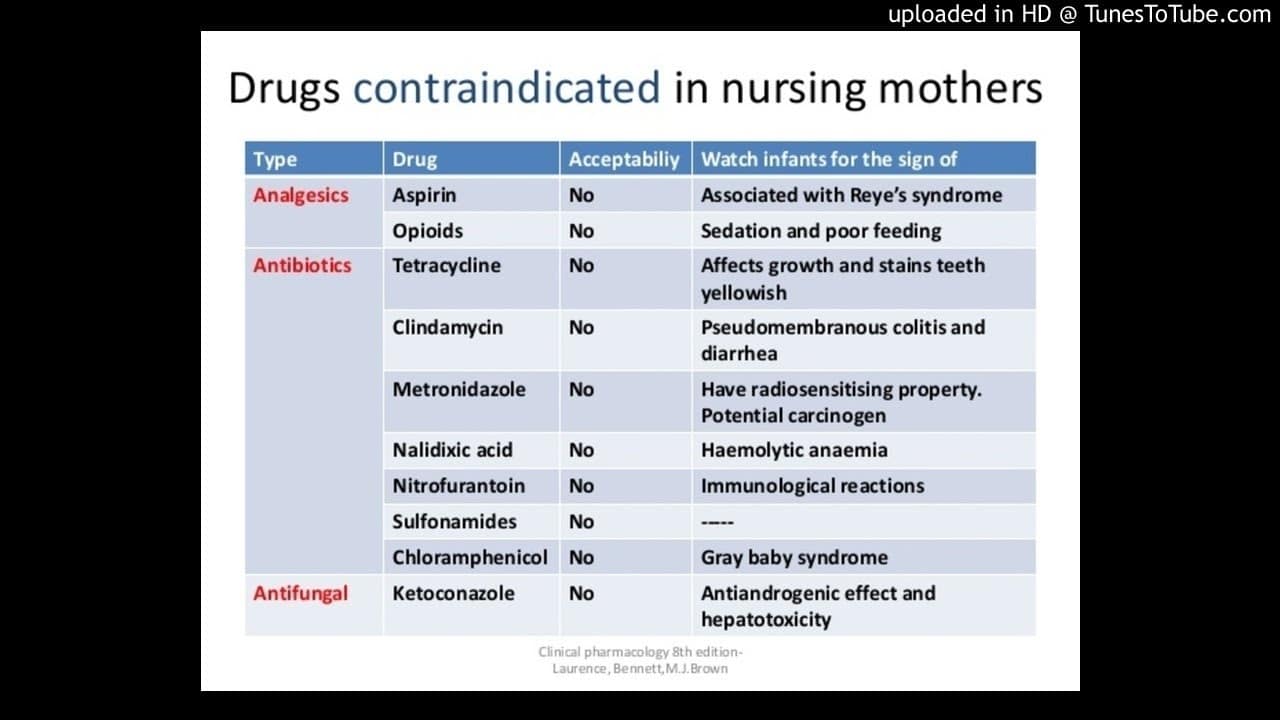
Medications that are not safe to take when breastfeeding:
Some drugs can be taken by a nursing mother if she stops breastfeeding for a few days or weeks. She can pump her milk and discard it during this time to keep up her supply. During this time, the baby can drink her previously frozen breast milk or formula.
These drugs include radioactive drugs used for some diagnostic tests like
- Gallium-67,
- Copper 64,
- Indium 111,
- Iodine 123,
- Iodine125,
- Iodine-131,
- Radioactive sodium, or Technetium-99m,
- Antimetabolites, and
- A few cancer chemotherapy agents.
There are drugs that if new mothers have to take them, they need to choose between taking them or breastfeeding.
Some of these drugs that should never be taken while breastfeeding include:
- Bromocriptine (Parlodel) - a drug for Parkinson's disease, it also decreases a woman's milk supply.
- Cyclophosphamide, Doxorubicin, and most chemotherapy drugs for cancer - these drugs kill cells in the mother's body and may harm the baby.
- Ergotamine (for migraine headaches)
- Methotrexate (for arthritis)
- Cyclosporine (for severe arthritis and psoriasis, aplastic anemia, Crohn's disease, kidney disease, and for after organ transplant surgery).
Drugs whose effects on nursing infants is not known but may be cause for concern include:
Antianxiety drugs
- Alprazolam
- Diazepam
- Lorazepam
- Midazolam
- Perphenazine
- Prazepam
- Quazepam
- Temazepam
Antidepressant drugs
- Amitriptyline
- Amoxapine
- Bupropion
- Clomipramine
- Desipramine
- Dothiepin
- Doxepin
- Fluoxetine
- Fluvoxamine
- Imipramine
- Nortriptyline
- Paroxetine
- Sertraline
- Trazodone
Antipsychotic drugs
- Chlorpromazine Galactorrhea
- Chlorprothixene
- Clozapine
- Haloperidol
- Mesoridazine
- Trifluoperazine
Other drugs
- Amiodarone
- Chloramphenicol
- Clofazimine
- Lamotrigine
- Metoclopramide
- Metronidazole
- Tinidazole
The above information is in part, information provided by the National Women's Health Center .
Another good resource for drugs during pregnancy is breastfeedingbasics.com.
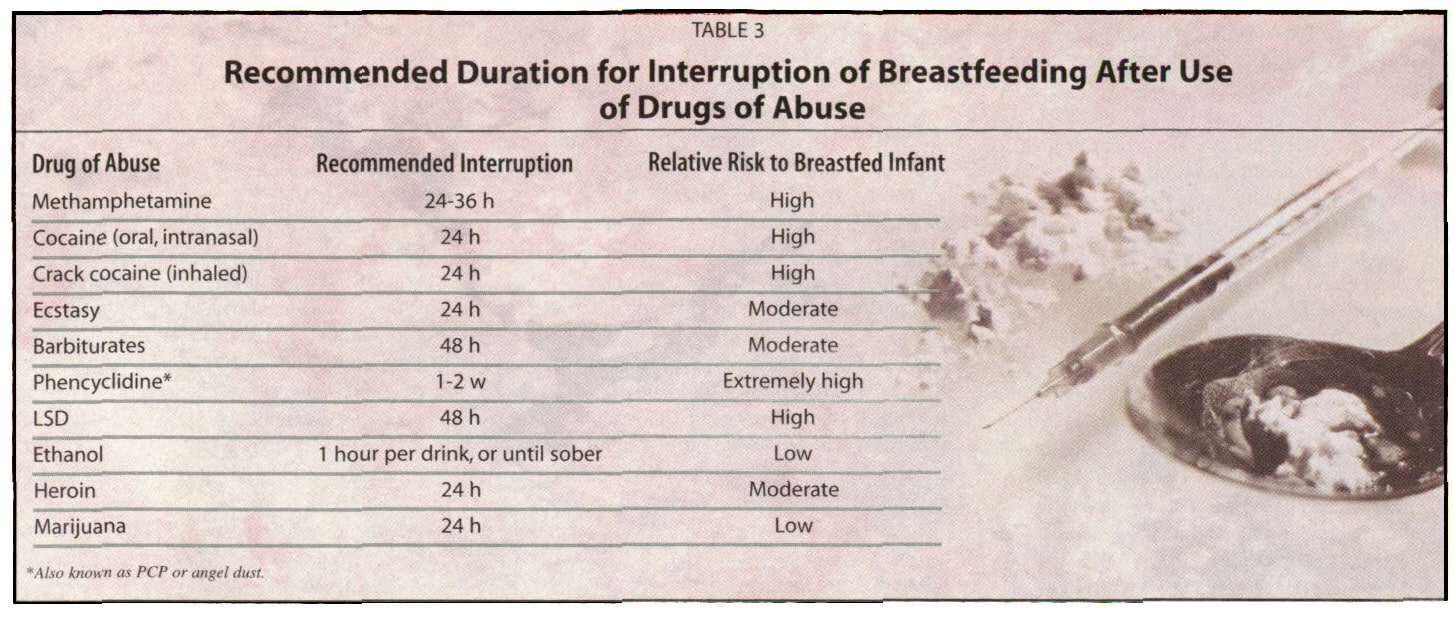
Recreational Drugs
While we all know that in an ideal world nursing mothers would be drug-free all the time, life happens, and mothers will smoke, drink alcohol or coffee, and partake on an occasional joint or stimulant.
What we should clearly understand, though, is the risks associated with these actions.
Smoking and nicotine
When it comes to smoking, avoid having the baby breathe second-hand smoke of any kind.
- Babies exposed to smoke have a higher incidence of respiratory illnesses, ear infections, and colic.
- Most importantly, they have a much higher risk of SIDs.
- While nicotine can be transmitted through breastfeeding, the important fact to note is babies absorb more nicotine from passive smoke than from the nicotine in breast milk
- Maureen Minchin (author of Milk Matters[1]) states: “Clearly, it is not ideal to smoke and breastfeed. But it is worse to smoke and not to breastfeed.” – just don’t smoke around your child.
Marijuana or Pot:
It’s a fact that nursing women who smoke marijuana transfer low levels of cannabis’ main psychoactive ingredient, THC, to their children via breast milk[2].
- The effect on child development remains unknown - The child dosage compared to an adult is small, but what impact it has on the developing brain is very unclear
- Studies in the past decade have greatly expanded knowledge about the endocannabinoid system and its role in healthy development – “Long-term microdose exposure of THC could disrupt that development,” said Kirane[3]
- Additionally, and as with nicotine, exposing your baby to second-hand smoke increases the amount of the drug the child receives
- But, as with cigarette smoking, as there is currently little evidence of harm, it is probably better to continue nursing if you smoke pot occasionally than to wean and deprive the baby of the proven protective benefits of breastfeeding. Just understand that this could change as the research results come in, and these decisions are always considered a risk assessment.
- Be aware though, marijuana can cause irritability, poor sleeping patterns, and in high enough doses, tremors, and vomiting.[4]
Alcohol:
Even though there is no evidence that occasionally consuming alcohol in moderation poses a risk for your baby, the safety of drinking alcohol during lactation is a subject of much heated debate.
Here’s how some experts weigh in on the topic:
- The AAP (American Academy of Pediatrics) considers alcohol compatible with breastfeeding. It lists some possible side effects of alcohol consumed in large amounts as drowsiness and weakness in the baby, and decreased milk production and inhibited let-down reflex in the mother, which may result in low weight gain.
- Thomas Hale (Medications and Mother’s Milk, 2012 ) states that “mothers who ingest alcohol in moderate amounts can generally return to breastfeeding as soon as they feel neurologically normal.” Rule of thumb: If you’re sober enough to drive, you’re sober enough to nurse your baby.
- Jack Newman (The Ultimate Book of Breastfeeding Answers) says “Reasonable alcohol intake should not be discouraged at all. As is the case with most drugs, very little alcohol comes out in the milk. The mother can take some alcohol and continue breastfeeding as she normally does. Prohibiting alcohol is another way we make life unnecessarily restrictive for breastfeeding mothers.”
Below are facts associated with alcohol and breastfeeding:
- Alcohol is passed to your baby through breast milk
- When a nursing mom drinks, the alcohol enters her bloodstream quickly, but only a small amount (less than 2%) transfers into her breast milk
- Peak concentration is about 30 to 60 minutes after drinking (60 to 90 minutes if it is taken with food)
- The effects of alcohol on the breastfeeding baby are directly related to the amount of alcohol a mother consumes.
- Moderate to heavy drinking (2 or more alcoholic drinks per day) can interfere with the let-down reflex and the milk-ejection reflex.
- It also can harm the baby's motor development and cause slow weight gain.
Caffeine:
The caffeine in five or less cups of coffee each day will not cause a problem for most nursing mothers and babies.
- less than 1% of the maternal dose is transferred to the infant.
- Peak levels of caffeine are found in breast milk about an hour after the moms ingests it.
- If you consume more than that, some babies will be fussy and over-stimulated.
Prescription Amphetamines:
Amphetamines usually prescribed for ADHD or narcolepsy when used in the prescribed dose are compatible with nursing. If you abuse them, they can accumulate in your milk, but even then, don’t usually cause problems for the baby.
Cocaine, Heroin, PCP (angel dust), and LSD:
The data is clear: they should never, EVER be used by nursing mothers, even in small doses.
They can and do cause serious medical problems in you and your baby. If you must abuse these drugs, don’t nurse your baby – and get some help.
The Facts:
- These drugs pass through breast milk and can make the baby high.
- Babies can become addicted to these drugs.
If you do use drugs such as amphetamines or heroin as a one-off, you will need to:
- Express your breast milk in the 24 hours afterwards and throw it away before you breastfeed again.
- Have a responsible adult to care for your children. It is not safe for you to care for or breastfeed your baby. You are not likely to be alert to your baby’s needs and could accidentally smother or drop your baby.
- Never sleep with your baby especially if you have been using drugs or alcohol.
For more detailed information about the safety of specific drugs during lactation, here are some resources:
The AAP (American Academy of Pediatrics) has published a statement called “The Transfer of Drugs and Other Chemicals Into Human Milk”. Because so many new drugs have come out during the past several years, many drugs currently in use have not been reviewed by the AAP and don’t appear on this list. Here’s a link to the AAP website where you can find more detailed information about the current recommendations.
An excellent resource for information about the safety of drugs during breastfeeding is Dr. Thomas Hale, an expert on drugs and breastfeeding. He is the author of a reference book called Medications and Mother’s Milk, and updates it every couple of years. It provides detailed information on drugs, including herbs, and includes useful information about the drug’s half-life, milk/plasma ratio, side effects, AAP ratings, and more. He also has a book called Clinical Therapy in Breastfeeding Patients (first edition) that gives an overview of medications that are useful for specific conditions. This is useful for doctors who are prescribing for lactating patients, especially because it gives alternative medications for different conditions.
It’s important to know that not all herbal preparations are safe to take while breastfeeding. While herbs are “natural”, they can be quite potent and cause serious side effects. For more information about herbs and breastfeeding, check out this article on Kellymom.
One helpful resource for nursing moms and their health care providers is Dr. Thomas Hale’s new InfantRisk Center. The InfantRisk Center provides up-to-date evidence-based information on the use of medications during pregnancy and breastfeeding. You can call them Monday-Friday 8am-5pm central time at (806)-352-2519, or visit their website.
Above all, remember that it’s almost always possible for a mother to continue nursing, even in the rare cases where temporary weaning is necessary. Remember how important breastfeeding is to you and your baby, and try to find a supportive health care provider who believes that nursing is as important as you do, and seek out a breast-feeding plan that fits with your situation.
Good Luck and Be Well
Disclaimer
ScuttleBugs does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on this Website or incorporated into it by reference. ScuttleBugs provides this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. We strongly encourage you to discuss your health needs with a health practitioner. If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
For more information about STIs, pregnancy, and breastfeeding, call the OWH Helpline at 1-800-994-9662 or contact the following organizations:
- Food and Drug Administration (FDA), HHS
Phone Number: 888-463-6332 - National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), CDC, HHS
Phone Number: 800-232-4636 - National Institute of Allergy and Infectious Diseases (NIAID), NIH, HHS
Phone Number: 866-284-4107 (TDD: 800-877-8339) - American Sexual Health Association (link is external)
Phone Number: 800-227-8922
Sources:
AAP. 2013a. Medications and breastfeeding. American Academy of Pediatrics. http://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Medications-and-Breastfeeding.aspx
AAP. 2013b. Serious illnesses and breastfeeding. American Academy of Pediatrics. http://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Serious-Illnesses-and-Breastfeeding.aspx
AAP. 2013c. When mom gets sick: Minor illnesses and infections while breastfeeding. American Academy of Pediatrics. http://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/When-Mom-Gets-Sick-Minor-Illnesses-and-Infections-While-Breastfeeding.aspx
American Academy of Pediatrics. 2013. Clinical Report. The transfer of drugs and therapeutics into human breast milk: An update on selected topics. Pediatrics 132(3):e796-e809. http://pediatrics.aappublications.org/content/132/3/e796.full [Accessed May 2016]
American Academy of Pediatrics. 2012. Policy Statement. Breastfeeding and the use of human milk. Pediatrics 129(3):e827-41. doi: 10.1542/peds.2011-3552. http://pediatrics.aappublications.org/content/129/3/e827.full [Accessed May 2016]
CDC. 2013. Lyme disease transmission. U.S. Centers for Disease Control and Protection. http://www.cdc.gov/lyme/transmission/
CDC. 2010. MV and congenital CMV transmission. U.S. Centers for Disease Control and Protection. Chttp://www.cdc.gov/cmv/transmission.html
CDC. 2009. Breastfeeding: Hepatitis B and C infections. U.S. Centers for Disease Control and Protection. http://www.cdc.gov/breastfeeding/disease/hepatitis.htm
Meier J, et al. 2005. Human cytomegalovirus reactivation during lactation and mother-to-child transmission in preterm infants. Journal of Clinical Microbiology 43(3):1318-24. http://jcm.asm.org/content/43/3/1318.full [Accessed May 2016]
NHS Choices. 2013. Treating for Lyme disease. National Health Service. http://www.nhs.uk/Conditions/Lyme-disease/Pages/Treatment.aspx
Breastfeeding: Lifestyle and Breast Milk
https://www.onhealth.com/content/1/breastfeeding_lifestyle_and_breast_milk
STD Aware
https://www.stdaware.com/blog/can-stds-pass-to-an-infant-through-breastfeeding/
CDC and breastfeeding
https://www.cdc.gov/breastfeeding/faq/index.htm
[1] http://infantfeedingmatters.com/
[2] https://journals.lww.com/greenjournal/Abstract/2018/05000/Transfer_of_Inhaled_Cannabis_Into_Human_Breast.5.aspx
[3] https://www.healthline.com/health-news/new-moms-who-smoke-pot-have-thc-in-breast-milk#4
[4] https://www.onhealth.com/content/1/breastfeeding_lifestyle_and_breast_milk
